QI: Getting Inside Quality Improvement Mindset
January 13, 2016 · Matt Brock
It’s one thing to promote your practice as a pillar of patient-centered care; it’s quite another to prove it. Transforming to a PCMH involves a major redesign of processes, workflows and care-team structure. But change doesn’t always equal progress. The only way to know for sure whether you’re meeting milestones is to measure.
Enter quality improvement, or “QI.”
What Is QI?
QI is the systematic and continuous method of examining processes and exploring changes that lead to better patient outcomes, better service and better professional satisfaction. It is not a destination.
“One of the mistakes that people make is to approach QI as a one-time thing, as in, ‘We solved this one problem, so let’s pat ourselves on the back and go back to seeing patients,’” says David Gans, senior fellow of Industry Affairs for Medical Group Management Association (MGMA). “The lesson we’re learning is that PCMH [recognition] is not something you get to and you just stop. It needs to be renewed. It’s a state of being.”
PCMH recognition programs require practices to demonstrate continuous QI, but—importantly—organizations that offer PCMH recognition, like NCQA, don’t dictate which improvements must be made. It’s the care team’s job to decide and document.
Practices can focus QI programs on one goal or many. Common areas of focus include patient access, coding accuracy, scheduling, wait times and disease management for a specific group of patients. “If you have patients who have issues with diabetes or hypertension, you can structure a continuous improvement program around those needs,” says David Meyers, chief medical officer for the Agency for Healthcare Research and Quality (AHRQ).
Data: The Cornerstone of QI
To identify targets for improvement and measure success, practices must collect, monitor and analyze clinical and demographic data on an ongoing basis. “To improve quality, you have to collect data and feedback continually and identify problems early,” says Gans.
EHRs and practice management systems provide data, along with checklists, alerts and predictive tools to help standardize care. They may also feature electronic prescribing and test ordering, which reduce human error and redundancy. But internal audits, satisfaction surveys and clinical performance measurements can also yield valuable insight on areas with the greatest potential for improvement.
To consolidate data and simplify analysis, many practices use an enterprise data warehouse, or EDW. These warehouses may be embedded into an EHR, but they can also be purchased as software to help organize data from multiple sources onto a single page, says Bobbi Brown, vice president of Financial Engagement for Health Catalyst, a consulting firm in Salt Lake City, Utah. “If your data are housed in one single source, and everyone is using the same sources, it helps a lot,” she says. “Being able to set up protocols or clinical initiatives and following through to make sure everyone follows those protocols seems easy, but unless you have a data warehouse, you can’t pull that information up quickly.“
Be Strategic
The adoption of a stable QI strategy is also key. According to the Safety Net Medical Home Initiative (SNMHI), which developed a framework for PCMH transformation, QI strategy provides the infrastructure and tools to plan, organize and monitor improvements.
Start by creating an organizational policy that outlines your quality goals and your process for identifying strategic QI priorities. Define roles and responsibilities, including who is on the QI committee and who is responsible for metrics. Finally, outline a process for organizing, monitoring and concluding improvement projects.
Practices can use any number of QI methodologies to implement change, including lean principles, which focus on customer service and creating value. Lean has long been used in other industries.
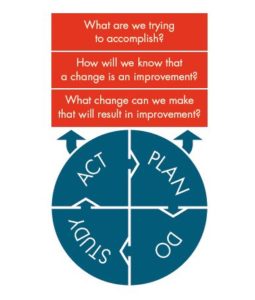
Among health care providers, however, the Model for Improvement, developed by Associates in Process Improvement, is often used. In essence, the model is a framework for managing the improvement process. It helps practices define what they are trying to accomplish, determine what actions they will take to effect change and identify whether those actions resulted in improvement.
The crown jewel in this method is the Plan-Do-Study-Act (PDSA) cycle, which allows organizations to test planned improvements in small steps.
That’s significant, says Gans. With PDSA, “You don’t do everything at once,” he notes. “It gives you a chance to say, ‘Is this going in the right direction?”
PDSA also allows you to recalibrate and start again. “The recalibration is critical because continuous improvement involves measurement, and measurement requires calibration,” says Meyers. “Are you collecting the right data at the right time?”
Think Beyond Clinical Outcomes
On the road to QI, physicians often excel at improving clinical outcomes—helping patients manage their blood pressure, ensuring that high-risk patients receive screenings and encouraging healthy patients to continue to get preventive care. But outreach to patients for immunizations and annual screenings, as well as care coordination with other providers across the healthcare continuum, frequently have room to improve, says Brown. EHRs can be useful tools in improving such measures, as they can be programmed to gather data about labs and tests that were ordered, indicate whether the patient completed them and display the results.
QI can also focus on assessing human factors, such as patient access, the patient experience and staff satisfaction. “Are [patients] satisfied with the care they received and do they feel good about your practice? How is your staff satisfaction?” asks Gans. Such metrics highlight other issues that may be prime candidates for QI initiatives.
QI Can Benefit Clinicians, Too
QI isn’t just good for payers and patients; it’s good for clinicians, as well. In an industry plagued by shrinking reimbursement and growing regulatory burdens, a shared vision for QI can reduce burnout and increase satisfaction. Having a real commitment to QI can “bring people back to the reason they went into medicine in the first place, which is to help,” Gans says.
As the health care industry evolves from volume-based to value-based, QI will likely assume a greater role. To survive and thrive, practices must be strategic about the changes they choose to make and committed to continuous improvement.
As the field matures, we’re seeing a lot more interest from the payer community in QI, and the way you’re going to demonstrate that you continue to show value is by continuous QI,” says Gans.